What is Diabetic Foot? Reasons? and Treatment Methods
The clinical condition that occurs with a foot wound caused by excessive pressure on the basis of ischemia (reduced blood flow) resulting from nerve damage and occlusive vascular disease that occurs as complications of diabetes, and the infection added to it, is called diabetic foot.
The clinical condition that occurs with foot wounds caused by excessive pressure on the basis of ischemia (reduced blood flow) as a result of nerve damage and occlusive vascular disease, which occur as complications of diabetes, and the infection added to it is called diabetic foot. One fifth of diabetic patients do not have to stand at some point in their lives. wound, ulcer or infection develops. In particular, diabetic foot accounts for 20 percent of the reasons why patients apply to the hospital. In addition, 50-70 percent of amputation surgeries are performed by patients with diabetes.
Causes of Diabetic Foot
There are two important causes of diabetic foot wounds: vascular occlusion and nerve damage. The organ most affected by nerve damage and occlusive vascular disease, which occur as complications of diabetes, is the patient's lower extremity.
Neuropathy is the leading cause of diabetic foot lesion onset. It has been understood that in most of the hospitalized patients, a physical factor that the patients are not aware of, such as hitting, hitting, stinging, burning, etc., initiated the wound. Patients often fail to recognize the injury at an early stage due to sensory loss and continue to stand and walk. This leads to progressive tissue damage.
The most important factor determining the outcome of diabetic foot ulcers, which are classified as neuropathic, ischemic and neuro-ischemic, is peripheral artery disease. Vascular damage in diabetic foot ulcers may occur in the form of macro and micro vessel involvement.
Common Risk Factors for Diabetic Foot
Common Risk Factors
Explanation
Peripheral Neuropathy
Numbness/insensitivity to sensory stimuli (such as cold, tingling, burning, touch) in the patient's foot. Pain may be observed starting from the fingertips and radiating towards the beginning of the limb.
Peripheral Artery Disease
Peripheral artery disease is defined as the blockage or narrowing of the arteries in the leg area. Individuals with diabetes are four times more likely to develop peripheral artery disease than those without diabetes. This rate increases depending on the duration of diabetes and age factors.
Infection
Symptoms of edema, bad odor and pus are observed as a result of infection in diabetic foot wounds. However, individuals may not feel the necrosis occurring in the skin due to numbness (neuropathy). Due to neuropathy, infection-based pain and temperature increases may not be felt.
Diabetes Duration
Another risk factor that affects the formation of diabetic foot wounds is the duration of diabetes.
Presence of other complications related to diabetes
The presence of other complications related to diabetes is also effective in the formation of diabetic foot wounds.
Choosing the Appropriate Shoes
Pressure applied to the bone protrusions in neuropathic feet with sensory loss may cause skin problems. As a result of choosing inappropriate shoes, the pressure applied to the area increases and this may cause skin ulcers.
Gender
Higher foot pressure in men compared to women causes a higher risk of ulcer formation in men.
Smoking
It is an independent risk factor for diabetic foot wounds.
Not paying attention to foot care health
Paying attention to foot care and performing it regularly is very important in preventing diabetic foot wounds.
Uncontrolled Blood Sugar Level
Another reason for the development of diabetic foot wounds is the lack of control of blood sugar levels.
Trauma
Due to the formation of neuropathy, patients cannot recognize small or large traumas. Repetitive traumas are a risk factor that may cause diabetic foot wounds, in other words ulcers, to become chronic.
Diabetic Foot Symptoms
● Skin color changes on the feet (bruising and blackening)
● Swelling in the foot or ankle
● Temperature changes (cooling) in the feet
● Pain in the feet or ankles when walking or at rest
● Permanent wounds on the feet
● Ingrown toenails
● Foot fungus
● Dry and cracked skin on the heels
● Signs of infection
As the diabetic foot infection progresses, it spreads to the bloodstream and causes a condition called sepsis, which can be life-threatening.
● Pain and redness in and around the foot wound
● Fever
● Tremors
● Weakness
● Very high blood sugar levels that cannot be controlled
● Advanced shock when intervention is delayed
Diabetic Foot Stages
In diabetic patients, the dryness of the feet caused by the impairment of the sweating mechanism due to autonomic neuropathy causes cracks, crevices and calluses on the skin. These cracks and crevices are susceptible to fungus and otherIt is the entry point for infectious agents. Infection causes cracks to grow and deepen. As a result of diabetes-related damage to the sensory nerves (diabetic sensory neuropathy), the patient does not feel the infected wound and pain on his foot. As the wound grows and the infection increases, and by the time the patient becomes aware of the wound with the discharge, the wound has already become threatening to the foot and leg. As a result of vascular damage due to diabetes, wound healing is delayed due to insufficient blood supply to the foot.
There are stages of diabetic wound. Diabetic foot stages are listed as follows according to the Wagner Classification:
● Stage 0: Healthy skin
● Stage 1: Superficial ulcer
● Stage 2: Deep ulcer
● Stage 3: Ulcer with bone involvement
● Stage 4: Forefoot (fingers/toe) gangrene
● Stage 5: Gangrene of the entire foot
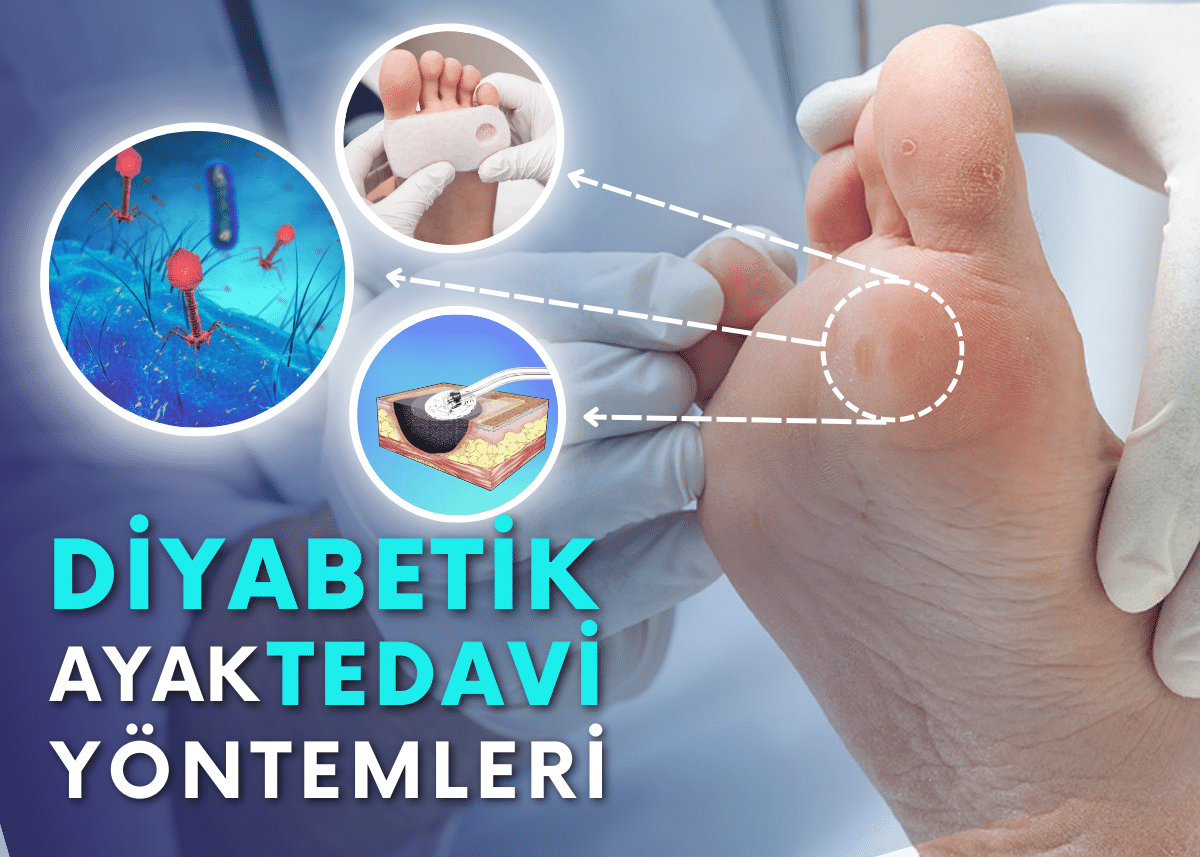
Diabetic Foot Treatment
In diabetic foot treatment, the current situation must first be fully revealed. First of all, it is necessary to reveal the risk factors that cause diabetic foot wounds and to create a treatment algorithm after classifying the wound.
1 Examination of peripheral vascular structure,
2 Presence of neuropathy
3. The spread of the existing wound and infection in the bone and soft tissue, especially bone tissue inflammation (osteomyelitis), should be questioned.
4 Detection of the microorganism causing the infection (there may be more than one factor) by appropriate isolation methods and initiation of antibiotic therapy
5 Wound care and dressing
6 Wound closure and reconstruction procedures
Treatment of Vascular Occlusion
Treatment of stenosis and occlusions in the leg veins due to diabetes can be done both closed (endovascular) and open (surgical).
Although problems can be seen in larger vessels in almost all patients with diabetic foot wounds, stenosis and blockages are definitely encountered in the small veins below the knee and in the feet. The vein that feeds the leg in the area below the knee divides into three and proceeds to the foot, and two of these veins unite in the foot to form an arch and network that feeds the entire foot and fingers. For wound healing, the treatments must provide blood supply to at least one vein that feeds the foot and fingers.
As a result of interventions made through needle holes in the groin and/or foot veins with closed methods called endovascular, foot nutrition can be provided in the angiography room without any incision.
● Balloon Angioplasty Method
● Vein Shaving Method
● Carbon dioxide (CO2) Angiography
● Surgical (By Pass) Method
Orthopedic Surgical Approach
Debridement is planned after evaluating the depth of the wound, if infection is present, which compartments it has spread to, and bone tissue involvement (osteomyelitis) using both physical examination and radiological imaging methods. The indispensable and most important part of wound treatment is debridement.
Debridement: It is the name given to the process of cleaning dead, dirty, infected tissues contaminated with microbes.
Debridement Methods:
Surgical (Sharp) Debridement
Larval Therapy
Enzymatic Debridement
Autolytic Debridement
Benefits of debridement:
● Removes necrotic/rough tissue and callus
● Reduces pressure on the wound
● Allows control of underlying tissues
● Helps drainage of secretions or inflammation
● Helps optimize the effectiveness of topical preparations
● Accelerates healing
Enzymatic Debridement
It can be achieved using a variety of enzymatic agents, including collagenase, papain, a combination of streptokinase and streptodornase, and dextrans.
Autolytic Debridement
It involves the use of dressings that maintain the moisture balance of the wound environment.
Thus, defense mechanisms (neutrophils, macrophages) can clean the tissues that have lost their vitality by using the body's enzymes.
Larval Therapy
It is a method in which fly larvae, known as green bottle flies, are used for biological debridement.
Antibiotic Treatment
Foot infections in diabetic patients require carefully selected antibiotic therapy in addition to debridement and wound care. Antibiotic selection is made according to the type of wound and laboratory results of the sample taken from the injured tissue. Treatment of diabetic foot infections should be started as soon as possible because the infection in the soft tissue can quickly spread to the deep tissues, making the treatment more difficult. Treatment duration varies from one week (for mild soft tissue infections) to 6 weeks (for osteomyelitis). Antibiotic treatment should be continued until the symptoms of infection improve.
Wound Care and Dressing
Diabetic foot wounds should be evaluated separately. The need for debridement should be evaluated for each dressing and dead tissue should be removed when necessary. First of all, during dressing, the wound should be washed with isotonic solution and the wound should be covered with sterile gases to keep it moist. The wound should not be wrapped too tightly and movement of the wound area should be restricted. There are different wound dressings that can be used depending on the current condition of the wound. As the condition of the wound changes, the dressing used may also change.
Wound Dressing Types
FILM COVER, TRANSPARENT FILM • The simplest covering, polyurethane structure, semi-permeable, protective for moisture balance. 1. On clean, exudate-free wounds awaiting epithelialization 2. On surgical incisions 3. On other products
2. ABSORBENT DRESSES • Basic dressings are used to absorb medium and large amounts of exudate. 1. HYDROCOLLOIDS 2. FIBER/ALGINATES 3. FOAMS
3. ABSORBENT (EXUDATE ABSORBING PRODUCTS) Hydrocolloids. They are mostly in cellulose structure. They consist of substances such as Gelatin, Pectin and CMC.
3. GELS, HYDROGELS • Provides moisture balance in the wound and helps autolytic debridement
4. ANTIBACTERIAL, ANTIMICROBIAL COVERS • Silver • Chlorhexidine • Silver Sulfadiazine • Iodine • Bismuth
Wound Closure and Reconstruction
In wounds whose infection has been treated and sufficient clean granulation tissue has developed, the existing wound is surgically reconstructed with partial skin grafting, local flaps or free flap surgical methods.
Pay Attention to the Following to Recognize Early “WARNING” Symptoms of Foot Problems
should be
• Redness, swelling or increased temperature in the foot or ankle
• Change in size and shape of the foot or ankle
• Pain in the foot while resting or walking
• Open wound, cut, blister, skin peeling, inflammation or non-healing wound
• Ingrown nail, nail thickening like a horn and showing deformity
• Redness, thickening and calluses on the skin, small round wound (like a bird's eye) in the middle of the callus.
FOOT CARE
● Cut your toenails straight across, do not cut the edges towards the nail bed and do not roll them, do not cut them deeply.
● Change your socks every day, wear wool or cotton socks instead of nylon
● If your socks have rough seams, wear them with the outside of the sock inside out.
● When you buy new shoes, wear the socks you always wear and never wear your shoes without socks.
● . Wash your feet every day using mild soap and warm water, check the temperature of the water with your hand and elbow before submerging your feet, and do not use very hot water.
● Check your feet daily for cuts, scrapes, fungus and possible blisters. If you have any redness, blisters, pain or swelling, calluses or rough skin, consult your doctor, get early treatment, do not self-treat.
● . After washing the feet, take care between the third and fourth and fourth and fifth toes and dry them with a soft towel.
● When you go to the doctor, you should definitely take off your shoes and socks and have your feet examined.
01 01
Diabetic and Charcot Foot Surgery
One of the procedures that people should pay attention to and follow is diabetic and Charcot foot surgery. Diabetic foot is a disease seen in diabetic patients who do not have good blood sugar control. With the persistence of health problems, people's quality of life decreases significantly. In this sense
diabetic and charcot. Diabetic and charcot feet, which can cause limb loss if left untreated, are diseases that should be taken into consideration.
Diabetic and Charcot Foot Surgery
One of the procedures that people should pay attention to and follow is diabetic and Charcot foot surgery. Diabetic foot is a disease seen in diabetic patients who do not have good blood sugar control. With the persistence of health problems, people's quality of life decreases significantly. In this sense, diabetic and Charcot foot surgery is of great importance.
What is Diabetic and Charcot Foot Surgery?
Most foot problems seen in diabetic patients are related to vascular occlusion, vascular stenosis or nerve damage. Charcot foot is a complication seen in neuropathic patients and is one of the most serious diseases. When left undiagnosed and untreated, it results in loss of the limb. In this case, bones break on their own and wounds occur on the foot due to the resulting deformity.
Redness and increased temperature in the feet are symptoms of Charcot foot disease. Many patients state that the complaints started after minor traumas. As the disease progresses, bony protrusions and joint instability that disrupts the anatomical structure and function of the foot may be observed.
In this case, diabetic and Charcot foot surgery is a branch of medicine used in the treatment of these diseases. It is very important for sick people to keep this condition under control as much as possible. Otherwise, as the health problem progresses, people's perception of the position of the joints in the foot deteriorates due to nerve damage.
What are the Symptoms of Diabetic and Charcot Foot Disease?
Although there are many symptoms of diabetic and Charcot foot disease seen in people, they vary from person to person. One of the important factors in the disease is to apply to the diabetic and Charcot foot surgery department if these symptoms are observed. Symptoms seen in patients are:
-Redness on the feet
-Swelling in the feet
-Increased temperature in the feet
-Ulcer on the skin
-Seeing bony protrusions
-Deterioration of the anatomical structure of the foot
-Disruption of foot function are some of the symptoms of diabetic and Charcot foot disease.
Redness, swelling and increased temperature in people's feet are the first symptoms encountered. It is necessary to pay attention to these symptoms. Because foot pain may not be seen at first. In some patients, symptoms begin with severe pain.
If the disease progresses, skin ulcers, bone protrusions and anatomical structure disorders may occur. If these symptoms are observed, you should immediately go to the diabetic and Charcot foot surgery department.
CONTACT US
 TR
TR  EN
EN  RU
RU .png)
.png)